It’s often said that breastfeeding your baby will just come naturally – after all, women have breastfed their children for thousands of years, right? But just because breastfeeding is ‘natural’ doesn’t necessarily mean that it’s easy. If you’re looking for a complete guide to help you through the ins and outs of your breastfeeding journey, then you’ve come to the right place!
Breastfeeding – especially if you are choosing to do it exclusively – can be hard, but there are countless benefits that come from nursing your child. The first few weeks of your breastfeeding journey will probably involve a steep learning curve, but once you and your little one settle into a rhythm, you’ll be able to handle mealtimes like a pro.
There’s a lot to learn about breastfeeding, but luckily, there is a lot of support available to help you through this unique time in your and your baby’s lives. Keep reading to learn all about the stages of breastfeeding, tips, and tricks to help you navigate common nursing problems, and how the choice to breastfeed can keep both you, and your little one, healthy.
Table of Contents
Why breastfeed?
Although breastfeeding is often thought of as the primary way for mothers to feed their newborn child, plenty of moms throughout history have used wet nurses, animal milk, and formula to keep their babies fed.
Currently, the medical community encourages breastfeeding as the superior form of food for babies. While modern formulas contain the same nutrients as breast milk, a mother’s milk can actually change in composition while a baby ages. This means that breast milk is essentially ‘custom-made’ for each baby and their individual needs.
Some other benefits of breastfeeding include:
- Time – Breastfeeding is incredibly handy if you’re in a hurry. You don’t spend extra time washing bottles or mixing up formulas.
- Safety – Especially in areas of the world with poor sanitation, breastfeeding is much safer than formula. With breastfeeding, you don’t need to worry about contaminated water or whether bottles have been properly sanitized.
- Health Benefits – Some studies have suggested a link between breastfeeding and improved infant and maternal health. Breastfed babies are at a lower risk of SIDS (sudden infant death syndrome), diarrhea, respiratory infections, and even ear infections.
It’s important to remember that even though breastfeeding comes with plenty of benefits, modern formula can be a wonderful substitute for some families. When you’re making the choice whether or not to breastfeed, it’s important to consider the needs of you, your baby, and your family.
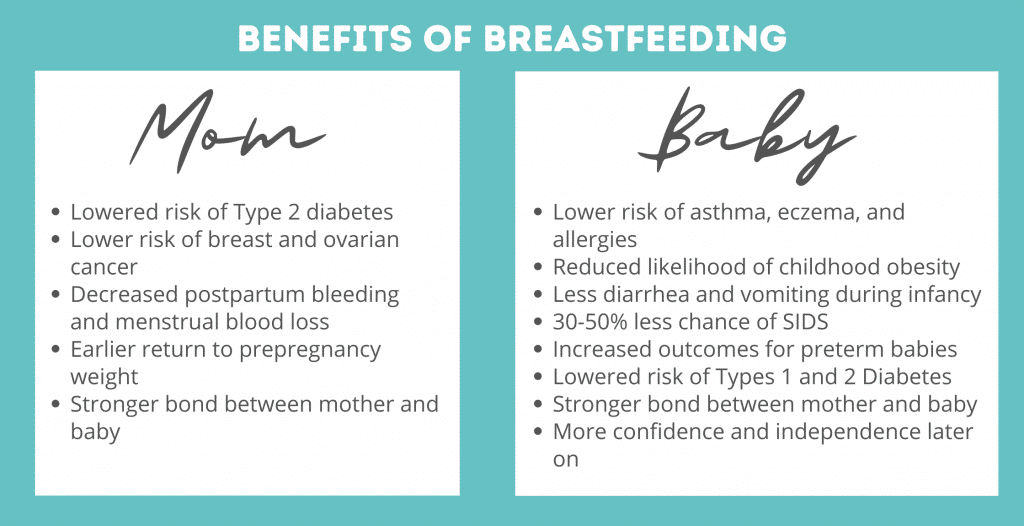
How baby benefits from breastfeeding
One of the people most likely to benefit from breastfeeding is obviously going to be the baby drinking breast milk.
Here are some of the biggest health benefits a baby might experience from breastfeeding:
- Lower risk of asthma, eczema, and allergies.
- Reduced likelihood of childhood obesity.
- Less diarrhea and vomiting during infancy.
- 30-50% less chance of SIDS.
- Increased outcomes for preterm babies.
- Lowered risk of developing Types 1 and 2 Diabetes.
Not only does a breastfeeding baby derive medical benefits from his mother’s milk, but there are plenty of emotional benefits to be gained as well.
Breastfeeding helps build a bond between a mother and her child – a bond reinforced by everything from the mother’s heartbeat to her smell. This bond can lead to a secure parent-child attachment that gives a baby more confidence and independence as he grows up.
How mom benefits from breastfeeding
Babies aren’t the only ones who benefit from breastfeeding; moms can cash in on the positives as well!
Some of the physical benefits mom might experience while breastfeeding include:
- Lowered risk of Type 2 diabetes
- Lower risk of breast and ovarian cancer
- Decreased postpartum bleeding and menstrual blood loss
- Earlier return to prepregnancy weight
There are plenty of nonmedical benefits a mom might also experience by breastfeeding.
Not only can nursing help strengthen the bond between mother and child, but it can also release positive hormones that decrease stress in the mother. Add in the fact that mom doesn’t have to wash bottles or mix up formula late at night, and breastfeeding can be a wonderful option.
Complete guide to breastfeeding
How do you know when your baby is hungry, or if they’re getting enough milk? What about that all-important latch, and different breastfeeding positions? How long and how often should you breastfeed? And what about pumping your milk?
Breastfeeding is a big term, and it can encompass everything from your milk first coming in after having your baby, to deciding when it’s time for your little one to wean.
Keep reading for a complete guide to the ins and outs of breastfeeding.
Understanding how your milk will come in
Most first-time mothers know that they’re somehow going to be able to provide milk for their baby, but very few know exactly how the process works.
There are actually several different stages of milk development: pre-birth preparation, colostrum, transitional milk, and mature milk.
Pre-Birth Preparation
There isn’t a sudden switch that flips and allows your body to suddenly make milk for your baby. The process is gradual, and your body actually begins preparing to nurse very early in your pregnancy.
Even as early as 5-6 weeks into the pregnancy, a woman’s breasts start to become fuller and more tender. As pregnancy progresses, a surge of hormones multiplies the milk ducts and gland-producing cells in the breast as the body prepares to produce milk. Most of the fat and supportive tissues that make up breast volume are replaced by glandular (milk-producing) tissue.
Most women are fully capable of producing breast milk as early as the end of the second trimester, so even if your baby is born early, you’ll be able to feed them.
Colostrum
The very first drops of milk you produce for your baby actually aren’t called milk at all. Instead, early milk is called colostrum, although you may hear some doctors refer to it as ‘liquid gold.’ That’s because colostrum is incredibly nutritious, and even a few drops can go a long way toward feeding your baby.
Colostrum is produced for the first 2-5 days after you give birth, and doesn’t look much like milk. Colostrum is extra thick, sticky, and is often yellow, clear, or white. The benefits of colostrum are even greater than those of more matured breast milk.
Colostrum can:
- Help build your little one’s immune system by introducing antibodies and white blood cells.
- Contribute to the protective coating of your baby’s digestive system.
- Help your baby pass their first poop.
- Prevent jaundice.
- Contain the perfect blend of nutrients for your baby.
- Prevent low blood sugar.
Most women only produce a few teaspoons of colostrum per day. Even though that may seem like a teensy amount, your baby’s stomach is only about the size of a marble at birth, so even a little colostrum can be plenty filling and contains all the nutrients your little one needs.
After a few days, your colostrum will begin to change into what’s known as ‘transitional milk.’
Transitional Milk
One of the coolest parts about breastmilk is that it changes along with your baby. 2-5 days after birth, your milk will go through its first change as it shifts from colostrum to what’s known as transitional milk.
This change is often referred to as a mother’s milk ‘coming in,’ and can feel like a sudden rush of fluid to your breasts. Your breasts will likely feel extremely full and heavy, and you may begin to leak milk (if you haven’t already!)
Transitional milk is a mix of colostrum and more mature milk, and this transition phase often lasts for about 2 weeks. Transitional milk has lots of fat, lactose, and vitamins, and also contains more calories than colostrum alone.
The extra calories are needed by your growing baby as he adjusts to life outside of the womb.
Mature Milk
After two weeks of change, your mature milk is finally ready to come in.
90% of mature milk is water, which keeps your little one hydrated. The remaining 10% of the milk is made up of fat, protein, and carbohydrates. Mature milk is actually split into two main types: fore-milk and hind-milk. Fore-milk is produced at the very beginning of a feeding and tends to be more watery and vitamin-heavy. In contrast, hind-milk is extra fatty and helps babies gain weight.
Even though your milk is technically ‘mature’ a few weeks after you give birth, it still goes through changes as your baby grows.
Breast milk can taste different depending on what mom eats, so if you eat garlic fries for dinner, your baby will be able to taste the difference in his milk a few hours later. And if you get sick, your breastmilk will incorporate antibodies which then pass on to your little one to keep him healthy.
Learning the signs of a hungry baby
Although you’ve spent nine months developing a special connection with your baby, you two still have plenty of things to learn about one another. And one thing you didn’t have to worry about when your baby was still comfortably settled in your womb? Trying to decide if she was hungry!
Even though they aren’t using words, yet, babies are still pretty good at communicating to you that they’re ready to eat.
Most newborns indicate they’re hungry by:
- Acting alert and active.
- Turning their head to search for the breast (also called rooting).
- Moving their fists to their mouth.
- Sucking on their hands.
- Smacking their lips.
- Opening and closing their mouth.
If your baby gets too hungry and is tired of waiting, she’ll probably begin to cry or fuss. It’s best to learn her hunger cues before she resorts to crying, though; not only will it save you a headache, but it can be hard for your crying baby to latch onto the breast and feed.
Getting baby to latch while breastfeeding
A ‘good latch’ is one of those ubiquitous breastfeeding terms that might not make much sense to a new mom.
The ‘latch’ refers to the way your baby takes your nipple in her mouth in order to breastfeed. If your baby has a hard time latching onto your breast, then it can make the process of nursing difficult, unsuccessful, or even painful.
A licensed lactation consultant can be invaluable when it comes to helping you and your baby perfect your latching technique. They can help troubleshoot your technique, and offer you tips specific to your own situation.
In general, a good latch involves three, basic steps:
- Rub your nipple across your baby’s lips. Your child will know that food is on its way, and open their mouth in anticipation.
- Use one of your hands to guide your nipple toward your baby’s mouth. Your nipple should be aimed slightly upward toward the roof of your little one’s mouth, and your baby’s chin should be facing outward rather than be tucked into her chest.
- Guide your nipple into your baby’s mouth. Your little one’s lips should rest around your breast and fully cover the entire areola. You should also notice a tight ‘seal’ between your skin and your child’s lips, and you may feel your baby’s tongue below your nipple. If the latch is shallow (your baby’s mouth just covers the very tip of your nipple or it’s painful) then you can put a clean finger between your breast and your little one’s mouth to break the latch and try again.
It’s normal for the first few days of breastfeeding to take some practice or feel uncomfortable. Make sure that you’re focusing on getting a good latch before feeding your baby, or else nursing may become painful.
Some signs that your baby has a good latch include:
- Nursing is comfortable and pain-free.
- Your baby’s head isn’t turned to the side or in a strange position.
- Your little one’s chin is touching your breast.
- Your entire breast is in your baby’s mouth, not just your nipple.
- Your baby’s tongue is beneath your breast and her lips are turned out against your skin.
- You can see or hear your baby swallowing as she feeds.
If you’re having a hard time getting your baby to latch, it’s important to stay calm and focused. It might help to move to a quiet place where you can really focus on getting the latch right.
Don’t settle for a painful latch – you should never be in excruciating pain while breastfeeding. If it is painful, you should get help from a lactation consultant.
How to handle a premature breastfeeder
If your child was born prematurely, it may be especially hard to help them latch well.
Preemies have much smaller mouths, which can make it tricky for them to get a good, deep latch. Premature infants also have less energy to draw milk from the breast, so you may find your little one drifting off before they’ve finished their meal.
You can try using a nipple shield to help your preemie baby latch on to the breast. In many cases, however, doctors recommend you pump or express your breast milk and feed it to your baby in a bottle until they’ve gotten a bit bigger.
The most important thing for premature infants is that they’re receiving adequate, consistent nutrition. If nursing from the breast just isn’t working, your child can still receive the benefits of breastmilk if you pump and feed it to them in a bottle.
The colostrum you produce for the first few days after giving birth can massively improve your little one’s outcomes, keep them healthy, and help them gain weight and strength.
How long should you breastfeed
When you first begin to breastfeed your baby, you may not know exactly how long to let them eat.
While each baby is different, most newborn breastfeeding sessions last about 20-45 minutes. It’s important to keep in mind that newborn babies are pretty sleepy, so you may need to encourage your little one to keep eating for a full session rather than sucking for five minutes, falling asleep, and then waking up hungry half an hour later.
Try feeding on the first side for a few minutes, or until your baby naturally stops suckling and seems sleepy and relaxed. After a quick burp break, you can try the other side, stopping again when your little one seems satisfied. Some babies will only eat from one side at a time, although most will nurse from both breasts at each feeding session.
How often should you breastfeed
You should breastfeed your newborn baby on-demand, which means that when your baby is hungry, you should feed them.
Most newborns will eat 8 to 12 times every 24 hours, although the timing isn’t always consistent. Your baby may eat once every hour during the day, but go three hours between feedings at night. Or your baby may ‘cluster feed,’ which means they’ll eat several times close together and then wait for a few hours before eating again.
Newborns should be fed at least every 3 hours, even if they seem extra-sleepy. New babies have very small stomachs, so they need to eat often in order to stay full. Keep an eye out for your baby’s feeding cues; they’ll help you know if your little one is hungry before it turns into full-blown crying.
Breastfeeding positions
There isn’t one single way to position your baby for breastfeeding, although there are some basic steps to follow to make sure you and your baby are comfortable while nursing.
When you’re ready to nurse:
- Make sure you’re in a comfortable position. This can be sitting up with pillows or an armrest to help support your arms and your baby, or lying down against pillows.
- Position your baby close to you, with her mouth and nose facing your nipple.
- Support your breast with a free hand so that it’s near your baby’s mouth, but not pressing against her chin.
- Latch your baby onto your breast by gently rubbing your nipple across her mouth and allowing her to take your breast into her mouth. If the latch feels shallow or is painful, use a clean finger to separate your baby from your breast and try the latch again.
Although these basic steps work for any position, there are a few nursing positions that work very well for breastfeeding mothers. Some positions work better in different situations than others, so it can be nice to practice with a few positions until you find one or two that work best for you and your baby.
Laid-Back (Biological Nurturing) Position
Often the first nursing position mothers will try, laid-back, or biological, nursing is a natural, easy fit for many moms and newborns.
- Lay comfortably in bed, on a couch, or on a recliner. Make sure you have some good pillow support for your head and lean back.
- Put your baby on your chest, and let her cheek rest near your bare breast. You can also rub your nipple on her lip to encourage your little one to open her mouth.
- Use one hand to maneuver your breast if you need, and your other hand to support your baby’s bottom or thigh. Don’t let your baby’s legs dangle in the air; she should be supported by your body.
Cradle Position
As your baby grows, the laid-back position may become uncomfortable or untenable.
Many mothers have great success with the cradle position since a nursing pillow is used to help support the baby’s increasing weight.
- Cradle your baby in your lap, with her lying on her side and you sitting up. Your baby’s body should touch the front of yours.
- Use a nursing pillow to lift your baby up to nipple height and help support your elbows and arms.
- Use one hand to support your breast, while your other arm cradles your baby against your chest.
- Guide your baby toward your breast and allow your baby to latch. Looking down, you should see your baby’s side, and her mouth should cover your entire nipple. Her shoulder and hips should be in a straight line, and her head and bottom should be level.
Cross-Cradle Position
If your baby doesn’t feel comfortable in the cradle position (or your arm just need a break), you may want to try a cross-cradle hold.
Cross-cradle is very similar to the cradle position, except that mom is cradling her baby in the opposite arm.
- Cradle your baby in your lap, with her lying on her side and you sitting up.
- Use a nursing pillow to lift your baby up to nipple height and help support your arms.
- Use one hand to support your breast.
- Your other hand should support your baby’s neck. Gently put your hand behind your baby’s ears and neck, with your thumb behind one ear and your index finger behind the other. The palm of your hand should fall between your child’s shoulder blades.
- Use your hand to guide your baby’s head toward your breast and allow your baby to latch.
Football (Clutch) Position
Newborns or mothers still recovering from a c-section may prefer a football position for nursing.
Just like it sounds, a football position tucks the baby into the crook of your arm along your side.
- Cradle your baby in your lap, with her facing you and you sitting up.
- Use a nursing pillow to lift your baby up to nipple height and help support your arms.
- Use one hand to support your baby’s neck, and tuck your baby’s legs and feet beneath your arm, almost as though you’re carrying a football.
- Use your other hand to support your breast.
- Guide your baby toward your breast and allow her to latch.
Side-Lying Position
When mom is recovering from labor (or just needs a break), the side-lying position can be a great way to relax while still feeding your little one.
While it’s a good way to allow mom to get to some sleep, someone should always be on hand to burp your baby and move her to a crib or bassinet once she is done nursing.
- Lie down on your side, with your baby lying on the bed facing you.
- Cradle your baby in your arm with her back against your forearm.
- Guide your baby toward your breast and allow her to latch. You can use pillows or blankets to help bring your baby up to nipple height if needed.
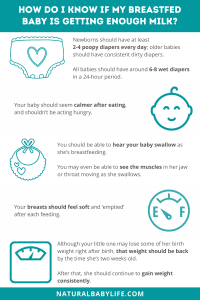
How to tell whether or not your baby is getting enough milk
Perhaps the trickiest part of breastfeeding is trying to tell whether your baby is actually eating enough or not. It’s not like bottle feeding where you can literally watch the liquid drain from the bottle.
While you may not be able to know exactly how many ounces your little one is drinking at each nursing session, there are a few ways to tell if your baby is getting enough to eat:
- Diapers – One of the best ways to tell how much your baby is eating is to see how much is coming out the other end. Newborns should have at least 2-4 poopy diapers every day, while older babies should have consistent dirty diapers. And all babies should have around 6-8 wet diapers in a 24-hour period.
- Swallowing – You should be able to hear your baby swallow as she’s breastfeeding. You may even be able to see the muscles in her jaw or throat moving as she swallows.
- Mood – Your baby should seem calmer after eating, and shouldn’t be acting hungry.
- Weight – Although your little one may lose some of her birth weight right after birth, that weight should be back by the time she’s two weeks old. After that, she should continue to gain weight consistently.
- Breasts – Your breasts should feel soft and ‘emptied’ after each feeding.
When to pump breastmilk
Although feeding straight from the breast can be a great option, some moms prefer to pump their breast milk and then feed it to their baby.
There are several situations that might make pumping breast milk a great alternative:
- If your baby was born prematurely, then pumping your milk can keep up your milk levels until your baby is able to breastfeed. And in the meantime, your baby can be fed your pumped milk out of a bottle.
- Pumping milk after your child finishes a breastfeeding session can help increase your milk supply. If you’re not producing enough milk, pumping can help rev up production. Or, if you’re trying to freeze milk for emergencies, pumping can help you produce enough milk to satisfy your baby while still preparing for the future.
- If you’re planning on returning to work but don’t want to switch to formula, you can choose to pump your breast milk. Pumped milk can then be fed to your baby by daycare workers or family members. Most employers are required by law to provide you with a quiet, private location for you to pump. The location must have an outlet so that you can use an electric pump, and you must be given time to pump throughout the workday.
- Some moms want dad to get in on the feeding action. Pumping some extra milk during the day means that dad can help feed the baby too, and can even switch off on the dreaded nighttime feedings.
Breastfeeding tips for every stage
You can begin breastfeeding your baby immediately after you give birth, although it may take some practice to really get into a rhythm with the process.
Your newborn will want to eat nearly all the time, which will give you both plenty of opportunities to practice. As your child gets older, she’ll nurse fewer times per day, and will eventually wean off the breast completely as she begins to eat solid foods.
On average,
- Newborns nurse on demand (8-12 times per day!);
- 1-2 month-olds nurse 7-9 times per day; and
- Exclusively breastfed infants nurse around 8 times a day until they wean to solid foods.
Preparing to breastfeed (while pregnant)
While you’re pregnant, your body will go through several changes in order to prepare for breastfeeding.
Here are some tips to help the breastfeeding process go smoothly:
- Invest in a good nursing bra – Look for supportive, underwire bras that are super-comfy. They’ll make your pregnancy more comfortable, and you’ll already have them when it’s time to nurse your baby.
- Take your prenatal vitamins – Those vitamins aren’t just for your baby; they’re for you, too! Breastfeeding your baby uses up a ton of your body’s nutrients, so it’s important you supplement with vitamins to keep your body running properly.
- Order a breast pump (or two…) – Even if you’re planning on just breastfeeding, things don’t always go as planned. Most insurance providers will completely cover the cost of an electric breast pump, and you can get a hand pump at most stores for less than twenty dollars. While hospitals will have pumps for you to borrow, you don’t want to get home with your baby and not have a backup plan for feeding him if you can’t get the latch right.
- Prepare for the unexpected – It’s good to have a plan for feeding your baby, but be aware that it may have to change. While breastmilk is a great food for your baby, the most important thing is that your little one is fed and healthy.
Breastfeeding at birth (and the first few days)
Once you begin breastfeeding, you’ll likely realize it comes with a steep learning curve.
Here a few tips to make getting started with the breastfeeding process a bit easier:
- Cut yourself some slack – You aren’t a bad mom if breastfeeding is tricky for you. There are so many factors at play, and even the most experienced breastfeeders have to start somewhere. It’s okay to practice and improve over time.
- Don’t be afraid to ask for help – Hospitals have lactation consultants who can come help you with any issues you might be having with breastfeeding. Take advantage of their advice! And even once you get home with your baby, if things aren’t working, don’t hesitate to ask for help or guidance.
- Use Lanolin! – One of the best nipple creams on the market is Lanolin, and is actually derived from sheep’s wool. It’s safe for you to put directly on your nipples, and you don’t even have to wipe it off before your baby breastfeeds. Lanolin protects your nipples and prevents cracking and soreness associated with the first few days of breastfeeding.
- Try different positions. There are plenty of ways to breastfeed, and one position might be the magic fit for you and your baby. Don’t be afraid to shake it up and try something new, especially at the beginning.
Exclusive breastfeeding
Once you’ve made it past the first curve, it’s time to settle into the long-haul.
Here are some tips to keep in mind once your baby is solely dependant on your breast milk:
- Trust yourself – You’ll probably always worry that your baby isn’t getting enough to eat, but trust that your body can keep up with demand. As your baby grows, you’ll automatically produce more milk to keep up.
- Set a schedule that works for you – Older babies can eat more consistently, and one day you’ll notice that you’ve fallen into a nice nursing rhythm.
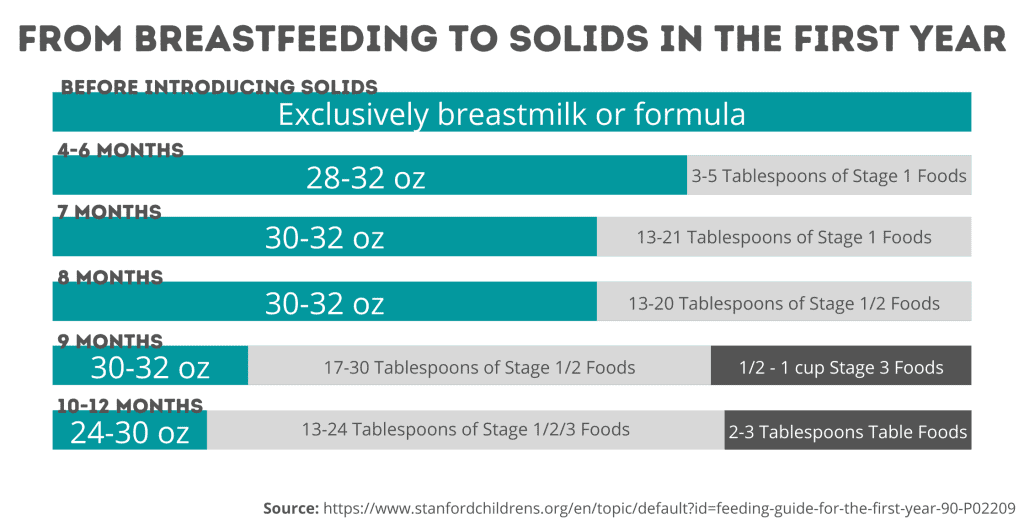
Breastfeeding when starting solids
Breastfeeding may change a bit as your baby starts solids. Suddenly, your milk isn’t the only source of nutrition anymore, and all those solid foods are nice and filling.
Here are a few things to keep in mind when introducing solid foods:
- Readiness – Don’t introduce solids until your baby is ready. He should be able to sit up in a high chair without help and should be grabbing things and bringing them to his mouth.
- Keep breastfeeding – Your child should still drink either breast milk or formula for their entire first year. Solid foods shouldn’t replace breastfeeding; at six months, your baby should just be testing out new foods that complement his regular breastfeeding schedule.
- Keep it about the same – Your baby’s breastfeeding schedule will probably stay pretty similar even after starting solids. As he gets older, you may notice he’ll nurse less frequently, but it will be a very gradual process.
Transitioning away from breastfeeding
Finally transitioning away from breastfeeding can be almost trickier than learning to breastfeed in the first place. You’ve built a great routine, and it can be hard to let that go. If you and your baby are still happy breastfeeding, there’s no reason to end it early – experts say that you can keep breastfeeding along with solid food for as long as you and your baby want.
If you’re ready to make the switch, though, it’s good to have a transition plan:
- Make sure it’s the right time to transition. Babies should drink only breastmilk or formula for their first six months, and then begin to slowly add solids until their first birthday. After that, they can drink cow’s milk, small amounts of juice, and water.
- Once your baby is old enough to transition, you should introduce a bottle or cup. Start with one bottle a day in place of a breastfeeding session. Most moms find it’s easiest to replace daytime feedings first, followed by naptime and morning feedings. And if your child is older than 6 months, you can skip the bottle and go straight to a cup instead.
- After 6 months, you can also replace breastfeeding sessions with solid foods. You can start with rice cereal mixed with some expressed breastmilk, and then work your baby up to chunks of food. The key is to gradually phase out your nursing sessions with solid foods and a bottle or cup.
Most babies transition away from breastfeeding at either the 6-month or 1-year mark, but plenty of families choose to continue breastfeeding for much later (or stop much earlier!) Each family is different, so don’t be afraid to do what’s best for you and your little one.
The most common issues moms encounter while breastfeeding
Although breastfeeding can be much less expensive and more straightforward than formula feeding, it comes with its own set of problems.
There are several common scenarios that most moms will have to deal with at least once during their breastfeeding journey, including clogged ducts, sore nipples, leaky breasts, an insufficient supply, and a poor latch.
Keep reading for info about each of these issues, and how to deal with them.
Poor Latch
Nothing hurts more than when your baby just can’t get a good latch on your breast.
Basically, your baby is sucking on just your sensitive nipple instead of on the larger areola. Your baby’s mouth should cover the nipple and most of your areola, and it shouldn’t hurt to nurse.
Practice is the best way to fix this problem, although help from a lactation expert can go a long way.
Clogged Ducts and Mastitis
Your breasts are made up of numerous milk ducts that allow milk to flow to the nipple for your baby. But sometimes, these ducts can clog and cause the milk to back up. Not only are clogged ducts painful, but they can lead to an infection called mastitis.
One of the best remedies for clogged ducts and mastitis is to keep nursing. Keeping the milk flowing will eventually unclog the duct and help clear up the infection. Warm compresses can help soften the clog, as can gently massaging the area while you’re nursing. You can also try cabbage leaves, which are a traditional home remedy for clogged ducts.
If you do develop mastitis, you should see your doctor. They can prescribe antibiotics that can help clear up the infection in a few days.
Sore Nipples
Most women will experience sore nipples at the beginning of their breastfeeding journey.
As you and your baby practice, the soreness should disappear until the process is painless.
Until then, you can use Lanolin or other types of nipple cream to help keep your nipples from drying out or cracking.
Leaking Breasts
This one is common, too: some women even have leaking breasts while they’re pregnant!
The best way to deal with leaking breasts is to nurse your baby often so that your breasts don’t become too full.
You can also use nursing pads beneath your bra to help soak up any excess milk that leaks between feedings.
Thrush
Thrush is a type of yeast infection that can appear as white or yellow patches inside your baby’s mouth.
Unfortunately, the thrush infection can also pass to a mother’s breast and cause burning and sore nipples. Thrush is treated with an antifungal medication, and if your baby has it then you should both be treated to prevent it from recurring.
Milk Supply
Some moms struggle with a low milk supply, while others have oversupply (too much milk). Both can lead to difficulties with breastfeeding.
Too little milk means your baby is going hungry, while too much milk means it’s hard for your baby to feed (it can be like drinking from a fire hose).
For mothers with low supply, pumping between feedings can help stimulate more milk production. And for mothers with oversupply, try holding your baby upright to nurse and use your fingers to reduce the flow of your milk to a manageable amount.
Potential medical considerations while breastfeeding
The AAP recommends that all women exclusively breastfeed their babies for the first 6 months after birth, regardless of any medical condition. The only listed reason a mother shouldn’t breastfeed is if she is infected with HIV, which can pass on to the baby through breastmilk.
With that being said, there are some factors to consider when deciding whether to breastfeed:
- Illness – Even though most illnesses can’t pass through breastmilk, if mom is ill, she can pass the sickness to her baby through close proximity (shared air in the case of the flu, for example). And some illnesses can make it hard for a mom to breastfeed by depleting her energy or even reducing her milk supply.
- Medications – Some medications can pass through a mom’s breastmilk and to her baby. While most pain relievers, antihistamines, decongestants, and even birth control pills are okay to take while breastfeeding, it’s important to discuss any medications with your doctor before taking them while breastfeeding. Most medications will also list on the label whether or not they’re safe for nursing women to take.
- Alcohol – Alcohol can pass to your baby through your breast milk. While the occasional glass of chardonnay is fine, drinking large amounts of alcohol right before nursing can affect a baby’s sleep patterns and development.
- Environmental Concerns – It is also possible for breast milk (even straight from the breast) to become contaminated with environmental pollutants, such as heavy metals and organics. If you’re worried your breast milk might contain pollutants, there are independent labs that can test your milk for signs of contamination.
Resources for breastfeeding moms
Breastfeeding can be hard, but luckily, there are plenty of resources that can help make it a bit easier:
Breastfeeding Courses
Most hospitals offer breastfeeding courses for new mothers.
There are also plenty of virtual or online courses that you can take:
- Lactation Link
- Milkology
- Medela Breastfeeding University (this one is free!)
Breastfeeding Support Groups
Sometimes, it’s most helpful to have people in your corner going through the same things you are.
Some of the most popular online breastfeeding support groups include:
- La Leche League
- KellyMom
- Milky Mamas Breastfeeding Support Group (on Facebook)
- The Leaky Boob (on Facebook)
And if you’re looking for more in-person help, check with your child’s pediatrician. They’ll be happy to recommend a lactation consultant who can come chat with you about your breastfeeding journey.