Trying to conceive is simultaneously terrifying and exciting, and also surprisingly complex. Everyone you know probably has a trick or method that they swear by, and it can be hard to discern science from old wives’ tales.
The most important things to keep in mind when trying to conceive are: begin taking prenatal vitamins at least three months in advance; check in with your doctor regarding your medications and health concerns; and track your cycle to find your fertile window either through a predictor kit or app, or by monitoring your basal body temperature.
Read on to learn about the steps you need to take before trying for a baby and all the tips you need to know to optimize your chances to conceive.
Table of Contents
An overview of conception and trying to get pregnant
Before trying to conceive, you should take a couple of steps to set you up for a healthy baby and your baby up for proper development.
Well before trying to conceive, mothers-to-be should check in with their doctors regarding any medications or supplements they are taking. Mothers with health concerns should consult their doctor regarding any health conditions they have to learn whether it impacts pregnancy or requires a change of management during the pregnancy. Your doctor will also be a great source of information if you have any specific questions about your health and pregnancy and trying to conceive.
Next, mothers should start taking prenatal vitamins at least three months before trying to conceive to maximize the benefits for the fetus. Prenatal vitamins come in many shapes and forms, and some are far superior to others.
Tracking your cycle and identifying ovulation maximizes your odds of conceiving. While it is normal to take 6 to 12 months to conceive, depending on the mother’s age, and determining your fertile window can make your efforts more productive.
What to do before trying to conceive
About 3 percent of babies in the United States are born with birth defects, and only thirty-four percent of women report taking prenatal vitamins three months prior to conceiving as recommended by doctors.
Preconception health and knowledge goes far beyond prenatal vitamins though. Being up to date on vaccinations, knowing and managing your medical conditions, and being aware of your cycle and fertile window are all the first steps that need to happen before trying to conceive.
Just as you will prepare a nursery for your new baby and buy them clothes and diapers for when they come home, so too is preparation important for conception. Unfortunately, we as a country lack the cultural common knowledge regarding conception health that we do about nursery preparation.
Healthy checkup
Your doctor can counsel you regarding the risks of any long-term medications you take and help you weigh the risk versus the benefit. Checking in with your doctor prior to trying to conceive will give you time to change your medications or try alternative treatments before you get pregnant. Your doctor may also recommend lifestyle changes, like the cessation of smoking or alcohol consumption.
Being honest with your doctor regarding your medical conditions is important, and no issue is too small. Some health conditions require special management during pregnancy, and that preconception visit is the perfect time to put that need on your doctor’s radar and make a plan to enact as soon as you get a positive test. For example, some thyroid conditions require a different medication dosage when pregnant, and delays in that change can lead to miscarriage.
During that appointment, you can also discuss preconception testing for you and your partner, which is especially important if either of you has a record of genetic conditions in your family. Doctors can order blood tests that conduct genetic screens to see if you two are both carriers for any of the same diseases, like cystic fibrosis.
Your doctor can also educate you regarding vaccinations, and either administer or refer you for vaccination if you need any boosters or other immunizations. Depending on the last time you were tested and the results, doctors will also recommend a Pap smear and STD testing.
The goal of a preconception visit is to ensure that your body is healthy and able to support both you and the baby during any pregnancy, and if not, help you find a path to work toward that point.
Prenatal vitamins
The importance of prenatal vitamins cannot be overstated, and they are actually recommended for continuous consumption by all women of childbearing age, regardless of intention to get pregnant. Those trying to conceive should start taking prenatal vitamins at least three months before attempting conception.
Common defects that become less likely with sufficient Folic Acid are spina bfida, which causes lifelong paralysis, and encephalopathy, which causes death, usually within 3 days of birth. Recent research also indicates that early prenatal vitamin usage can lower the risk of Autism in high-risk families.
Prenatal vitamins provide extra vitamins and minerals to support the growing fetus, but what sets prenatal vitamins apart from a general multivitamin is the emphasis on quality Iron and Vitamin B9 (more commonly known as folate or Folic acid). Iron supports the development of the placenta and fetus while Folic acid drastically reduces the chance of the fetus having neural or spinal cord defects.
When choosing a prenatal vitamin, be aware that most over-the-counter prenatal vitamins have Folic acid rather than folate. Folic acid is the synthesized alternative to folate and is most commonly found in processed foods as a supplement. Folate is found in whole foods like leafy greens.
The difference is important because a large portion of the population, as high as 60 percent by some estimates, lack the ability to process Folic acid into the needed active folate, methylfolate. People who cannot metabolize the Folic acid miss out on the health benefits to the fetus. The ability to process Folic acid into active folate is based solely on genetics, so it is ideal to seek out supplements with folate to ensure full Vitamin B9 absorption.
When purchasing prenatal vitamins, remember that they are covered as a no-cost prescription under the Affordable Care Act. Your insurance may require a prescription from your doctor before covering them.
If you are interested in getting over-the-counter prenatal vitamins, here are a few suggestions:
- Gentle Prenatal Vitamins with Folate – This vitamin is a special low-nausea formula that includes ginger and Vitamin B6 to help curb nausea. These are also totally vegetarian.
- SmartyPants Gummy Prenatal Vitamin – These are one of the most popular prenatal vitamins because it comes in chewable gummies rather than capsules. It does include folate
- Pink Stork Liquid Prenatal Vitamin – This liquid prenatal can be mixed with your morning beverage and is especially beloved by women experiencing extreme nausea.
| Image | Title | Price | Prime | Buy |
|---|---|---|---|---|
 Top
Top | Gentle Prenatal Vitamins with Natural Folate (Methylfolate - MTHFR Safe), Low Nausea Formula | PrimeEligible | Buy Now | |
 Top
Top | Daily Organic Gummy Prenatal Multivitamin: Probiotic, Vitamin C, D3 & Zinc for Immunity, Biotin, Omega 3, Selenium, Methyl B12 for Energy | PrimeEligible | Buy Now | |
 Top
Top | Pink Stork Liquid Prenatal Vitamins: Organic Whole Food Blend + Folate + Iron + Zinc + Vitamin C + Elderberry + Biotin | PrimeEligible | Buy Now |
Product prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.
Prices pulled from the Amazon Product Advertising API on:If you do get a prenatal vitamin with only folic acid, get a separate methylfolate tablet to take in conjunction with it.
Monitoring ovulation and finding the fertility window
To intentionally try to conceive, there are a number of physical and biological cues that women can monitor to find their most fertile window and time intercourse.
Because all women’s cycles vary, and there’s even variation from month to month for each woman, it is important to understand each phase of a menstrual cycle and the different methods for identifying the phases.
Ovulation is the release of an oocyte (egg) from a woman’s ovaries, which happens once during a menstrual cycle. The egg travels down the Fallopian tube, and if it is not fertilized, menstrual bleeding (a period, or menstruation) occurs as the uterus sheds its lining because a fertilized egg did not attach.
Ovulation is one of four phases of the menstrual cycle
A woman’s menstrual cycle is the period of time from when bleeding begins during one cycle until bleeding begins again to initiate the next one. The average cycle length is 28 days, but anywhere from 21 to 40 days is considered normal. A cycle is divided into 4 phases, with menstruation being the first.
After menstruation (the menstrual phase) ends, the follicular phase begins. This phase is named after the follicles in the ovaries that will release an egg. The pituitary gland in the brain releases a hormone called the Follicle-Stimulating Hormone (FSH) that causes 5 to 20 follicles to form. Each follicle houses an immature egg, and usually only one reaches maturity and is released. More rarely, multiple eggs may be released and twins conceived.
The developing follicles release estrogen, and the estrogen triggers the pituitary gland to release Luteinizing Hormone (LH). The LH triggers the release of a mature egg in the phase called ovulation. FSH and LH are the hormones used to predict ovulation.
The egg then travels down the corresponding Fallopian tube, and it lives for approximately 24 hours. It ceases to exist if it is not fertilized by sperm.
During the luteal phase, a fertilized egg may attach to the uterine lining to create a pregnancy. The follicle that housed the egg releases progesterone and estrogen to maintain the uterine lining to give any fertilized egg a chance to implant. If no fertilized egg implants, menstruation will begin about 14 days after ovulation, and the cycle repeats.
Why is it important to track ovulation when trying to conceive?
Because an egg only lives for about 24 hours, the window of conception is finite, and because every woman’s body is different, the window of conception is very variable.
Tracking ovulation will help you conceive more quickly. Rather than blindly having intercourse throughout a cycle, you can identify your fertile window to maximize your chances of conception.
Tracking can also help you identify when you are having troubles conceiving, and the data from the methods described below can help your doctor recommend next steps.
Ovulation predictor kits
Ovulation predictor kits (OPKs) help you determine your fertile window via testing the LH levels in urine.
You will be testing to find your LH surge, which indicates that ovulation has occurred or is imminently occurring. There are a few different varieties out there depending on your budget and stomach for plastic waste.
Some tests, like those by ClearBlue, look exactly like traditional plastic pregnancy tests and give you a smiley face when it detects a high enough level of LH.
Others are just tiny strips that you dip into your urine, and the test line gets progressively darker as more LH is in your urine. These tests are much less expensive and allow for frequent testing to most accurately track your LH surge.
| Image | Title | Price | Prime | Buy |
|---|---|---|---|---|
 Top
Top | Clearblue Early Detection Pregnancy Test, 2ct | PrimeEligible | Buy Now | |
 Top
Top | AccuMed Pregnancy Test Strips, 25-Count | PrimeEligible | Buy Now |
Product prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.
Prices pulled from the Amazon Product Advertising API on:What you should know before relying on OPKs
Because OPKs rely on the level of LH present in your urine, it is possible to miss the surge that indicates ovulation if you only test once per day. These tests do not provide ‘real-time’ LH levels.
You can increase your information about your cycle, and therefore increase your chance of best timing intercourse, by using OPKs in conjunction with the other methods described below.
Ovulation predictor apps
Ovulation predictor apps allow you to input information into the app, and it churns out recommendations for the best days to try to conceive.
Information that you input varies from app to app, but may include basal body temperature, cervical mucus observations, photos of your OPK, and any physical symptoms you are having.
For example, Glow relies on information supplied by the user regarding the heaviness of flow each day of a period, daily physical symptom reports, and daily basal body temperature reports to customize a calendar that provides days that are low, medium, or high fertility. You can also upload photos of your OPK strips, and the app also takes into account the darkness of the test line to predict ovulation.
Another great app is the Fertility Friend. While its bland name and clunky platform may not instill a lot of confidence upfront, this is an example of a time you should not judge a book by its cover. It relies on the same information input as Glow, but it churns out very detailed charts and grafts that you can use to track your own cycle or take to your doctor if you think it is time to get some additional input.
Some companies bundle LH test strips and an app to give one comprehensive product. One such is Modern Fertility, which sells test strips specifically meant to be uploaded into their app for customized predictions.
Finally, a similar option to the bundles above is to purchase devices that are meant to read the LH strips, and those devices generate ovulation predictions in the corresponding app. Mira is the leader in this technology.
| Image | Title | Price | Prime | Buy |
|---|---|---|---|---|
 Top
Top
Top
Top | Modern Fertility Ovulation Kit - 20 Ovulation Test Strips in Each Ovulation Predictor Kit. Free iOS App. | PrimeEligible | Buy Now | |
 Top
Top | Easy@Home 50 Ovulation Test Strips and 20 Pregnancy Test Strips Combo Kit, (50 LH + 20 HCG) | PrimeEligible | Buy Now | |
 Top
Top
Top
Top | Mira Fertility Tracking Monitor Kit with 10 Ovulation Test Wands and Connected App | PrimeEligible | Buy Now |
Product prices and availability are accurate as of the date/time indicated and are subject to change. Any price and availability information displayed on [relevant Amazon Site(s), as applicable] at the time of purchase will apply to the purchase of this product.
Prices pulled from the Amazon Product Advertising API on:Measuring basal body temperature
Basal body temperature is your body temperature when you are fully at rest.
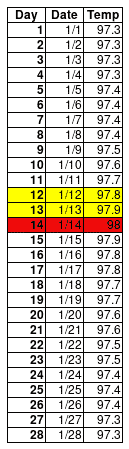
A woman’s body temperature slightly rises during ovulation, and then if implantation occurs, it stays elevated. Noting this body temperature rise can help you confirm that ovulation occurred, so, if tracked over a number of months, it can also help you predict when it usually occurs during your cycle.
Your basal body temperature must be taken vaginally before you get up in the morning. Several thermometers are available specifically for this purpose, and many will automatically transmit your information to an app on your phone.
Taking your basal body temperature and recording it, known as charting, can be challenging because your temperature can be influenced by illness, poor sleep, alcohol, shift work, oversleeping, and more. If you’d like to try and chart your temperature, click here to download a helpful spreadsheet.
One way to make it less burdensome is to wear an ovulation monitor, like the Ava bracelet, that tracks your body temperature overnight and sends the information to an app.
Calendar method
The calendar method is the least reliable method for tracking ovulation because it is not customized. Instead, it assumes that ovulation will occur 14 days before the next predicted period start date.
For women with perfect cycles, the calendar method is by far the easiest and least invasive method.
Changes in cervical mucus
Your cervical mucus changes throughout the course of your menstrual cycle thanks to the changes in hormones through each phase. Monitoring this cervical mucus can give you another clue to your fertile window.
To do this, insert two clean fingers into your vagina, and examine any substance that comes out on your fingers. It can be hard to understand what you are seeing in isolation, so you should check your cervical mucus every day that you are not having menstrual bleeding.
Leading up to ovulation, the mucus will be sticky and tacky, and it won’t stretch if you stick your thumb to your fingers and then separate them. Right before ovulation, you may see an increase in the volume of mucus, and the mucus will be slippery or like egg whites. Ideally, it will stretch when you separate your thumb and fingers.
This egg-white cervical mucus helps sperm survive longer in the reproductive tract, giving you the best chance at conceiving. If you see a lack of cervical mucus, fertility doctors recommend increased water intake and some supplements. You can also bring this up with your own doctor.
Professional help
After using the above methods to chart your cycle for a few months, if you are not successful, you can ask your doctor for assistance in determining your fertile window and for feedback as to whether there is anything abnormal in your charting that indicates a need for further investigation.
The general recommendation is that it is “normal” for a woman under 35 to take up to 12 months to conceive. Women 35 and older should ‘only’ try for six months before seeking help. However, if you are employing all the methods above for several months and notice a pattern in your cycle that seems abnormal, reach out to your doctor sooner.
Your charting can indicate that your luteal phase is too short to allow for implantation or that ovulation is not occurring. Rather than continuing to put yourself through the wringer of months of trying when you suspect something is wrong, pull in a professional to give customized input. Maybe a chat with your doctor will help put some worries to rest and make your days a bit easier.
Regular OB/GYNs can order hormone tests at specific points in your cycle if there are particular concerns. Some will refuse to do any fertility testing, and it will be up to the patient to pursue it elsewhere.
That type of testing can be very expensive if you have not met your deductible; $1,000 is a fairly common amount. If you are feeling concerned but are not ready to invest that money with a doctor, Modern Fertility offers at-home fertility hormone testing. They send you a kit for a finger-prick blood test that you mail back to their lab.
From there, they send you a customized report with your different hormone levels and where they fall in the range of normal. Modern Fertility offers several resources to help you learn about your results and always encourages that you show them to your doctor for further care.
Tips for her to increase odds for conception
Everyone’s mother and brother will have tips for you if you mention you want to get pregnant. Here are a few that are actually based on science rather than luck.
Ideally time intercourse
When trying to conceive, have sex every other day.
Sperm can live in the reproductive tract for 2 to 3 days if fertile cervical mucus is present. Eggs only live 24 hours, so the sperm should be waiting on the egg.
Be the healthiest you
A healthy egg is the most important determining factor in conception success, followed by healthy sperm and right timing. The key period for egg development is 90 days before the egg ovulates, so before trying to conceive, make the lifestyle changes recommended by your doctor.
Scientists agree that all signs point to nutrition being an important factor for both egg health and implantation.
Elevate your pelvis after intercourse
Whether this is an old wives’ tale or the real deal is still to be seen. A recent study of women who received intrauterine insemination found no increase in pregnancy rates among women who remained lying down versus those who got up and moved around. Some doctors will recommend it, and others tell patients not to waste their time. Ultimately, though, if it gives you peace of mind to try something that doesn’t hurt or cost anything, then it is worth it.
Don’t worry about relaxing
The old adage of ‘just relax, and it will happen,’ is not only false but harmful. Worry will not prevent you from getting pregnant. Worrying about how much you worry is not a burden you should put on yourself.
Limit chemical exposure
Chemicals in our homes and food and things we touch and put on ourselves daily can all impact both male and female fertility. BPA in plastics has received top billing in the news the last few years, but it is also found on recipes. Chemicals in makeup, deodorants, scents, and even soaps can act as hormone disruptors and reduce your odds of conception.
“It Starts with the Egg” by Rebecca Fett is considered the seminal work on this topic that is digestible for anyone who is not a medical professional.
Tips for him to increase odds for conception
The pressure and lifestyle changes should not only be on the woman. Men can also enact several lifestyle changes to increase the odds of conception.
Wear loose-fitting underwear
Boxers are the ideal underwear for men trying to conceive. Tight-fitting underwear reduces both the quantity and quality of sperm.
Do not masturbate in the fertile window
When trying to conceive, male ejaculations during the possible fertile window need to take place inside the female partner’s vagina.
The ideal period of abstinence prior to ejaculation is 2 to 3 days to ensure optimal sperm count and volume. Waiting longer can translate to greater numbers of dead or immobile sperm.
Be the healthiest you
Several lifestyle changes can create the best possible conditions for sperm:
- Decrease or limit alcohol use. Overuse can lower testosterone and, consequently, lower sperm count.
- Maintain a healthy BMI. Higher BMIs are linked with decreasing sperm counts and motility.
- Don’t smoke. Men who smoke have lower sperm counts.
- Avoid toxins. They can also lower sperm count
- Don’t use lubricants unless it is specifically “fertility-friendly.” Lubricants, including saliva, impede the movement of sperm.
- Keep the scrotum cool. Increased temperatures impede sperm production. Avoid hot tubs, saunas, and laptops on laps.
What if none of these things work?
Trying to conceive can change from fun and exciting to stressful and scary as the months wear by with negative after negative.
Unfortunately, it can also take a lot longer than television would have you believe, and for some people, no amount of trying and tracking and healthy eating will yield a baby without medical intervention.
Don’t be afraid to reach out to your doctor sooner rather than later
The general recommendation is that it is “normal” for a woman under 35 to take up to 12 months to conceive. Women 35 and older should ‘only’ try for six months before seeking help. However, if you are employing all the methods above for several months and notice a pattern in your cycle that seems abnormal, reach out to your doctor sooner.
After using the above methods to chart your cycle for a few months, and you are not successful, you can ask your doctor for assistance in determining your fertile window and for feedback as to whether there is anything abnormal in your charting that indicates a need for further investigation.
Your charting can indicate that your luteal phase is too short to allow for implantation or that ovulation is not occurring. Rather than continuing to put yourself through the wringer of months of trying when you suspect something is wrong, pull in a professional to give customized input. Maybe a chat with your doctor will help put some worries to rest and make your days a bit easier.
Regular OB/GYNs can order hormone tests at specific points in your cycle if there are particular concerns. Some will refuse to do any fertility testing, and it will be up to the patient to pursue it elsewhere.
That type of testing can be very expensive if you have not met your deductible; $1,000 is a fairly common amount. If you are feeling concerned but are not ready to invest that money with a doctor, Modern Fertility offers at-home fertility hormone testing. They send you a kit for a finger-prick blood test that you mail back to their lab.
From there, they send you a customized report with your different hormone levels and where they fall in the range of normal. Modern Fertility offers several resources to help you learn about your results and always encourages that you show them to your doctor for further care.
You can go straight to the experts
Many women report the unfortunate experience of wasting precious time by relying on the OB/GYN for advice or treatment, only to be referred to a reproductive endocrinologist months or years down the road.
You do not need your OB/GYN’s permission to consult with a fertility expert, called a reproductive endocrinologist, unless required by your insurance. The vast majority of fertility clinics will see you for a consultation if you simply call them.